In the previous article on this topic I discussed what heart disease is and who is affected by it.
In this article I want to focus on the signs and symptoms of heart disease, as well as risk factors, biomarkers, and how the disease is diagnosed.
I mentioned previously that heart disease is caused primarily by high levels of blood cholesterol, and that its usual endpoint (a heart attack) usually occurs in those aged 50 – 70.
So what are the symptoms of heart disease? Because heart disease (atherosclerosis) occurs gradually and over a long time it can often be a silent disease – just like limescale building up in the plumbing of a home it can go unnoticed until something catastrophic happens (a leak or a flood in the plumbing example, a potentially fatal heart attack in a human). Unfortunately, for some people the first symptom can be a heart attack. There are however some other signs and markers we can watch out for. If atherosclerosis has occurred in the heart arteries people can often experience angina – a pain in the chest described as similar to indigestion, as well as breathlessness. This occurs due to reduced flow of blood to the heart and a lowering of the heart’s pumping ability. Other symptoms can include pain in the neck, abdomen or back, pain, numbness, weakness or coldness in the extremities (always check with your doctor if you experience new, persistent or unusual symptoms).

But, you don’t have to wait for these symptoms to have a good idea of your heart and cardiovascular health. Other things like biomarkers and risk factors can give us an indication of what is going on in our arteries.
Biomarkers are Biological Markers – signs that can be detected through medical tests, like a blood test for example, that predict, or are associated with, a certain condition or disease. For example in diabetics (and in screening for diabetes) some biomarkers can be the person’s blood glucose level (the concentration of sugar / glucose in their blood), or their HbA1c level (Glycated Haemoglobin – the amount of haemoglobin in our red blood cells that has become attached to sugar molecules). Biomarkers can be extremely useful in detecting disease which would have otherwise gone undetected until more serious effects became noticeable.

In heart disease there are a number of biomarkers we can check in a simple blood test which can indicate conditions that may lead to heart disease. The primary biomarkers in heart disease detection are:
- Blood Total Cholesterol level
- LDL Cholesterol level
- Triglyceride level
- C-Reactive Protein (CRP)
- Homocysteine
All of these markers can give an indication of what is going on in the blood vessels and have been associated with (predictive of) heart disease in numerous studies of large amounts of people.
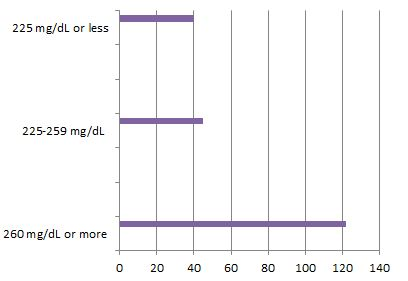
Of the useful biomarkers for detecting heart disease total cholesterol and in particular LDL cholesterol are probably the most consistently associated with heart disease. What does this mean? When a person has elevated LDL cholesterol in their blood they are far more likely to have the physiological process of atherosclerosis formation in their arteries – IE they are likely to have heart disease progressing silently in their blood vessels. In the previously mentioned study – The Framingham Study – people with increasingly higher LDL cholesterol levels had the highest risk of having a heart attack. As peoples levels increased they were more likely to have advanced heart disease and for a heart attack to occur.
Apart from Biomarkers, and their utility for detecting disease, we have risk factors – these are identifiable factors in our lives that are known to contribute to the progression of heart disease.
The most common risk factors are:
- Being a Smoker
- Having High Blood Pressure (Hypertension)
- Having High Cholesterol (discussed above)
- Having a Sedentary Lifestyle
- Having Diabetes



So knowing the signs & symptoms, known biomarkers and risk factors we can begin to see if we are at risk of developing heart disease, and make certain modifications to reduce our risk.
We can attempt to stop smoking, try to lower our blood pressure through diet and lifestyle, increase our levels of activity through exercise and lower our risk of diabetes by losing excess weight and controlling our intake of free sugars and saturated fats.
I will emphasise here that of all risk factors LDL Cholesterol is the one factor that drives atherosclerosis and Heart Disease – reducing the other risk factors while failing to reduce LDL Cholesterol blood levels will still leave you with an elevated risk of heart disease. Lowering LDL Cholesterol, via either diet or medications, will reduce your total risk of heart disease the most. These other risk factors still matter and should be addressed, but LDL and Total Cholesterol should be the main targets for reducing in any effort to lower heart disease risk.
In the next article I will discuss in detail the dietary changes we can make to drastically reduce our risk factors and our overall risk, allowing us to maintain healthy hearts long into our futures.

